Causes and Treatments for Achilles Tendon Injury
| ✅ Paper Type: Free Essay | ✅ Subject: Physiology |
| ✅ Wordcount: 3074 words | ✅ Published: 18th May 2020 |
Background and Significance:
Tendons serve to connect bones with muscle or muscle with muscle, and they are very important because they allow us to perform many functions and without them we would lose almost all of our motor capabilities. In this proposal, one specific tendon is targeted, the Achilles tendon. Tendons has can either be torn or ruptured, and the Achilles tendon is commonly injured in many athletes. This would be devastating because it restricts a person’s use of their legs because they can no longer put any support on the ankle region. This proposal aims to make an attempt at forming a scaffold with bioactive agents to try to increase cell proliferation for this large tendon to reduce recovery time. To achieve this, Interface tissue engineering will be used. It can be defined as: working towards the regeneration of tissue interfaces and ultimately enabling soft tissues to fix themselves. One example of this is grafts which are used in orthopaedic surgery and sports medicine. In addition, issue engineering aims to use scaffolds, cells, and specific chemical agents in order to attempt to restore the function of the tissue. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3260008/ )
If you need assistance with writing your essay, our professional essay writing service is here to help!
Essay Writing ServiceThis field is extremely important because of all its applications to modern medicine. By improving upon this science, we can find ways to speed up the healing process of injuries that would otherwise take extended periods of time to heal, which can range from a couple of weeks to several months. Scientists in this field have worked to increase the natural growth of tissues through the use of scaffolds, bioactive agents, and mechanical stimulation.
This proposal will focus specifically on repair of the connective tissues within the Achilles Tendon. The Achilles tendon connects the calf muscle to the heel bone (calcaneus) which makes it a very important tendon since it allows for our legs and feet to perform all the functions that it’s capable of. When this tendon tears, which means the tendon is damaged but still connected, or it ruptures, the tendon is split into two pieces that are completely separated, this can limit the person’s movement significantly. This type of injury is very prevalent when there is an increase in physical activity without stretching the tendon initially to get it accustomed to a sudden large need for its use. If the tendon is exposed to too much pressure all of a sudden, this can increase the risk of damage if not careful. It is very important to find ways to increase the repairing of this tendon in order to reduce the amount of time that a person must live with very restricted movement.
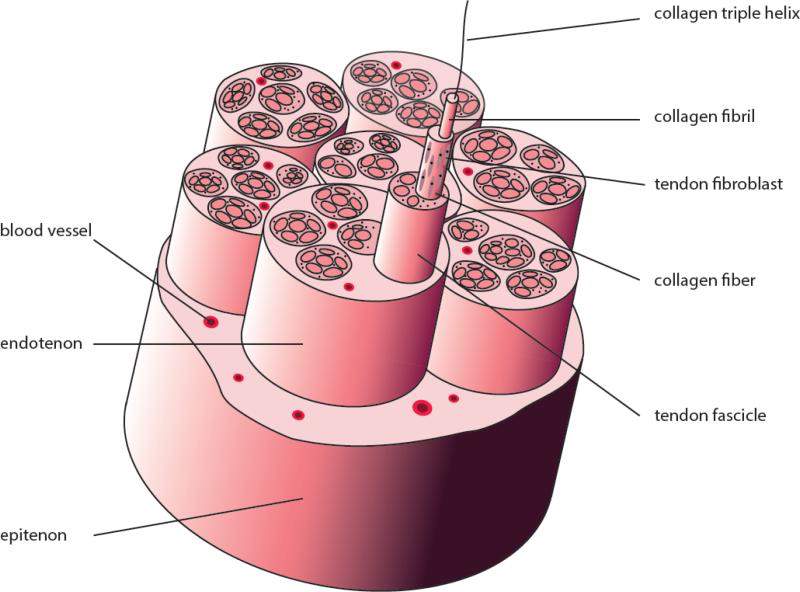
The tendon has a simple structure that consists of multiple strands of connective tissue which are made up of collagenous fibers. These collagen fibers are also made up of collagen fibrils. There are groups of tertiary, secondary and primary bundles of these collagen fibers distributed throughout the tendon and they are then wrapped around by endotenon, (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4041869/ ) which allows for all the bundles within the endotenon to move against each other while to tendon stretches during general movement. There is also the paratenon, which allows the tendon to move with other tissues without being disturbed. In addition, there are two types of cells within the tendons, the fibroblasts and fibrocytes. The fibrocytes are more matured cells and are typically tethered to the collagen fibers. The fibroblasts are immature cells that will eventually become the fibrocytes but start off away from the collagen fibers and instead are key to fast growth of collagen as well as the extracellular matrix. This structure is fairly simple, however, due to the fact that certain technology and techniques weren’t in practice before, it took awhile to figure out the specific functions of each component of the tendon’s structure. In order to accurately describe the structure, research was put into finding a tendon-specific lineage marker. One specific marker that proved to be very useful was the Scleraxis which aids in seeing the maturation of tenocytes and progenitor cells
. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4041869/ )
(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4041869/ )
During the natural healing process that occurs when a tendon either tears or ruptures, there are multiple steps within the process that occur. During the phase that follows immediately after the rupture of tendon. The surrounding area becomes inflamed and thus releases chemicals that attract cells such as neutrophils and phagocytes. Once the debris is disposed of through phagocytosis, the prolific stage begins and the tendon lays down a disorganized collagen matrix. The collagen is formed by the tenocytes from the tendon. The collagen is thinner in diameter in comparison to the original collagen in the tendon before the need for repair. The collagen fibers then increase in tensile strength and join together and get ready for a very long and slow healing process. The way that the fibers connect together makes the resulting repaired tendon much weaker when compared to the original strength of the tendon, making it important to find out ways to try to retain the strength and ability of the native tendon.
Typically when someone suffers from an Achilles tendon injury, they are told to rest and are given an orthopedic cast to help heal naturally and this can take a couple of weeks, however, when the tendon is ruptured, there is a need for the surgery and this healing can take up to a few months. There are a few different types of methods that can be used to help increase the cell proliferation and thus heal the tendon faster. One such method would be the use of a scaffold. Scaffolds can be of three different types: native tendon matrices, synthetic polymers, and derivatives of naturally occurring proteins. They help in providing structure to the tendon in order to promote faster growth of tenoblasts and tenocytes. In addition there are also bioactive molecules that can be used as growth factors in order to increase the growth of the tendon cells in order for more collagen to be produced so that the tendon can be rebuilt to connect the tendon back to its original form. However, with all of these methods, the tendon does not repair itself to the same strength as its original tendon, making it weaker after injury.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4041869/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4380768/
https://advances.sciencemag.org/content/4/10/eaat4537
Hypothesis:
I believe that the connective tissues within the Achilles tendon will have an increase in growth through the use of scaffolds and bioactive agents and will thus take a shorter period of time for the tendon to repair itself.
Aims:
- Promote the growth of the achilles tendon through a scaffold made up of a Tecason P plastic integrated with IGF-1 and TGF-B growth factors for its ability to mitigate inflammation when the tendon gets ruptured. The scaffold is included in order to provide structure and allow for the tendon to both retain tensioned as well as allow for the tendon to repair over this scaffold.
Materials and Methods:
Before this experiment can be performed, there are a few things that need to be set up in order to set up the specific groups. This includes both the setup of the bioactive agents that are going to be used as well as the creation of the scaffolds that will help in the repair of the Achilles tendon. It is important to make the bioactive agents in a specific way in order to maintain consistency across multiple samples and to make sure that there are no problems with the manufactured product. In addition, the same goes for the scaffold.
Our academic experts are ready and waiting to assist with any writing project you may have. From simple essay plans, through to full dissertations, you can guarantee we have a service perfectly matched to your needs.
View our servicesIn the case of this proposal, the type of scaffold that will be used is one that is 3d, has a tendon-like structure and through physical anisotropy can be microarchitectural manipulated. These types of scaffolds have proven to be effective because when tenocytes were introduced in vivo, phenotypic markers were expressed, showing that it is very effective when applied to tendons, or environments that emulate tendons. So, in order to produce such a scaffold, nanofibers need to be electrospun in order to produce a scaffold that has dimensions that can be manipulated at the microscopic level. In addition, this will allow for the scaffold to have pores that are also microscopic in order to accompany the needs of the tenocytes in the tendon tissues or the tissue culture. The machine needed to do this would be a electrospinning machine which functions through the difference of charge across the machine that attracts the negatively charged liquified material to make strand that are several nanometers in width. This allows for the most accurately made scaffold. After the electrospun mesh was formed, it was subject to laser perforation to make very small sized pores. This resulted in a uniform surface that had pores and non-pores equally spaced out. The core of the scaffold also will show a very complex structure that is essential for integrating the bioactive agents into the scaffold.
The bioactive agents are made in a different manner. They are made by taking the liquid bioactive agents, in this case IGF-1 and TGF-B growth factors, and are encapsulated in encapsulation matrices to prevent it from being contaminated and damaged by the external environment. Most growth factors are very diffusible and thus they can be imbedded in scaffolds, such as the ones made in this proposal. The method that can be used to integrate the two growth factors would be the use of genetic fusion to bind the natural polypeptides (growth factors) with the nonnatural polypeptides. The TGF-B growth factor will bind directly with the scaffold and the IGF-1 will bind with the cell culture to promote growth initially when the tissue culture is first introduced in the environment and when the tenocytes of the tissue bind with the scaffold. This allows the tissue cells to grow and multiply faster in two stages.
Some alternate methods that can be used for this experiment would be to use genetic fusion just with the use of natural polypeptides, however, this method wouldn’t be as efficient because it would require additional steps to make the polypeptides be able to combine with the scaffold. Therefore, the method of just combining natural and nonnatural polypeptides together is more effective and takes a shorter amount of time.
The experiment would first be tested in a separate environment that contains the two growth factors and the scaffold to facilitate the growth of the tissue culture. There would be multiple groups to see if consistent results are obtained. In addition another group will be tested on the tendons on live mice to see if they have the same effects in a more complicated environment.
The expected results of this experiment would be that when the tissue culture is placed in a petri dish, or a mouse, with the two growth factors and the scaffold the growth would start very quickly, but noticeable results would take a range of a couple of hours to a couple of days to become noticeable. Although it would show the results, this doesn’t necessarily emulate the same environment that would be in a human which is much more complicated than that of a mouse or an environment that is provided by a petri dish.
Some pitfalls that are possibly present in this experiment is that growth factors are very diffusible most of the time and thus are also unstable and can be unreliable at times. Therefore, the results can be inconsistent or just false from the beginning. In addition, although many efforts that can be made to ensure that the mice will accept the scaffold and growth factors into their bodies, there is still the risk that the mouse’s immune system can still reject the scaffold and can result in the immune system attacking it and compromising all of the results.
References:
- Ratcliffe, A., Butler, D. L., Dyment, N. A., Cagle, P. J., Proctor, C. S., Ratcliffe, S. S., & Flatow, E. L. (2015, March). Scaffolds for tendon and ligament repair and regeneration. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4380768/
- Tada, S., Kitajima, T., & Ito, Y. (n.d.). Design and synthesis of binding growth factors. Retrieved June 10, 2019, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3382770/
- Wang, Z., Lee, W. J., Koh, B. T., Hong, M., Wang, W., Lim, P. N., . . . Thian, E. S. (2018, October 01). Functional regeneration of tendons using scaffolds with physical anisotropy engineered via microarchitectural manipulation. Retrieved June 10, 2019, from https://advances.sciencemag.org/content/4/10/eaat4537
- Yang, G., Rothrauff, B. B., & Tuan, R. S. (2013, September). Tendon and ligament regeneration and repair: Clinical relevance and developmental paradigm. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4041869/
Other References:
- https://www.osapublishing.org/oe/fulltext.cfm?uri=oe-27-10-14457&id=412170
- https://www.tandfonline.com/doi/full/10.1080/03008207.2016.1231180?scroll=top&needAccess=true
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5221413/
- http://orion.bme.columbia.edu/lulab/pdf/Lee_2016_review.pdf
- http://bebevida.pt/ficheiros_artigos%5CMarx%201998%20oral%20and%20maxillafacial.pdf
- http://kqwww.fmmu.edu.cn/upload/htmleditor/3.pdf
- https://bpspubs.onlinelibrary.wiley.com/doi/pdf/10.1038/sj.bjp.0704372
- 2003hydrogelsreviewbiomaterials.pdf
- https://www.pnas.org/content/97/21/11307
- https://arxiv.org/pdf/1710.04392.pdf
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6067679/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4629810/
- https://academic.oup.com/rb/article/5/4/197/5035357
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5986909/
- https://thorax.bmj.com/content/thoraxjnl/74/2/164.full.pdf
- https://www.researchgate.net/profile/Luke_Olsen2/publication/330169762_The_skeletal_muscle_fiber_a_mechanically_sensitive_cell/links/5c320b14299bf12be3b30492/The-skeletal-muscle-fiber-a-mechanically-sensitive-cell.pdf
- https://www.researchgate.net/profile/Andrea_Bonetto3/publication/331309398_Bone_and_Muscle/links/5c8a57d6299bf14e7e7b73d5/Bone-and-Muscle.pdf
- https://www.ahajournals.org/doi/full/10.1161/JAHA.118.010456
- https://synapse.koreamed.org/DOIx.php?id=10.4196/kjpp.2019.23.2.141
- https://stemcellsjournals.onlinelibrary.wiley.com/doi/full/10.1002/stem.319
- https://www.sciencedirect.com/science/article/pii/S136970211170058X

(https://www.osapublishing.org/oe/fulltext.cfm?uri=oe-27-10-14457&id=412170)
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allDMCA / Removal Request
If you are the original writer of this essay and no longer wish to have your work published on UKEssays.com then please:
 GBR
GBR 












